[ad_1]
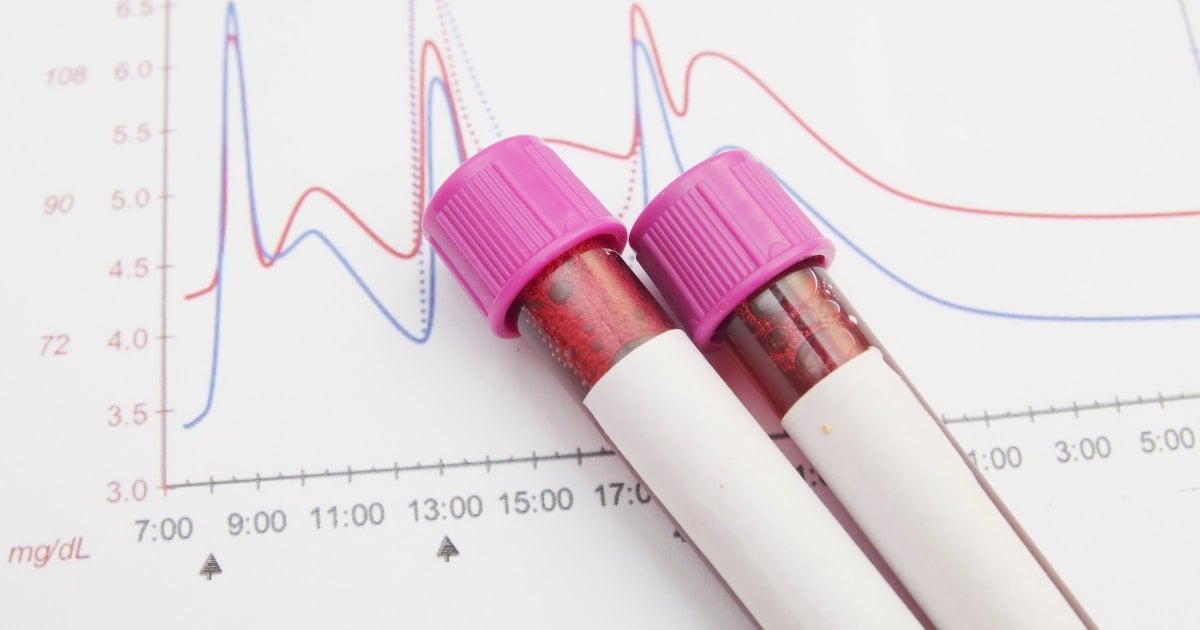
Figuring out what your blood sugar should be, as well as what is considered “normal,” can be confusing, especially if you have diabetes.
Blood sugar goals, or targets, can be different for everyone, and to make matters even more complicated, they can be different depending on the time of day.
This article will help you make sense of target blood glucose and A1c levels for both people with and without diabetes.
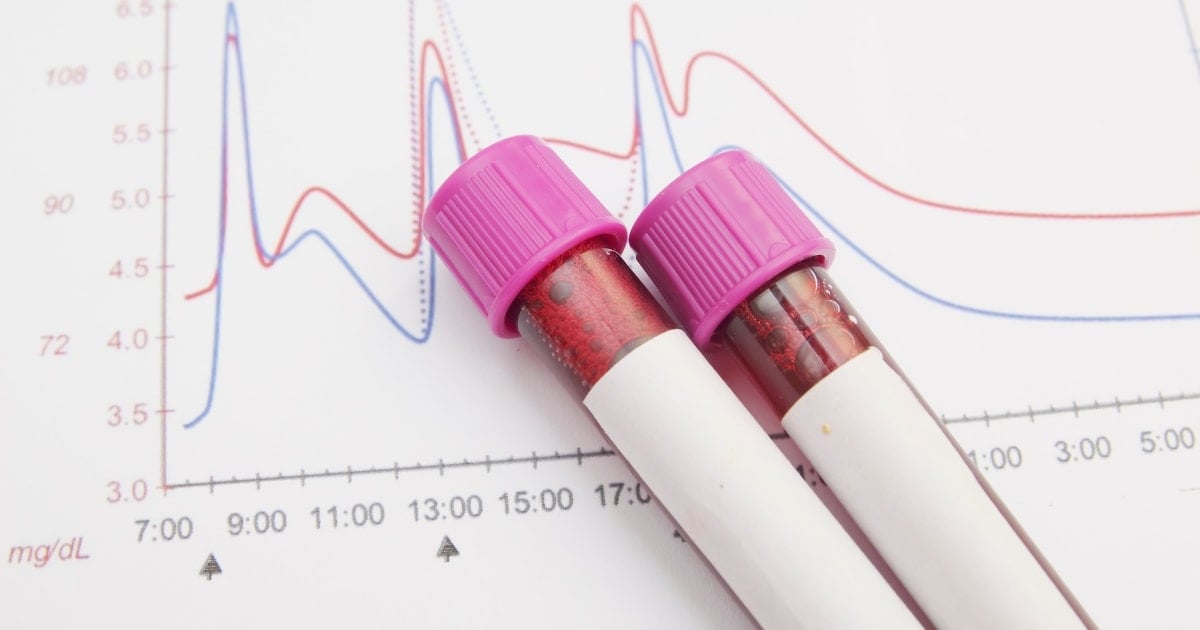
Table of Contents
Blood sugar and A1c chart: normal and diabetic blood sugar ranges
Learn more: What Are Normal Blood Sugar Levels?
What is blood sugar?
Blood sugar, also called blood glucose, is the sugar found in your blood. This type of sugar is the main source of energy, or fuel, for the body. It’s also the primary source of energy for the brain.
When you eat, the body breaks down the carbohydrate (carb) in food into glucose, which then is released into the bloodstream. As glucose levels in the blood begin to rise, the pancreas releases insulin, a hormone, to move glucose into cells to be used for energy.
How are blood sugars controlled in people who don’t have diabetes?
In people who don’t have diabetes, blood sugar levels are very tightly controlled in the body by two hormones: insulin and glucagon. Any extra glucose in the blood gets stored as glycogen in the liver.
When the body needs extra glucose for fuel, say, during exercise or overnight when you’re sleeping, glucagon signals the liver to release glucose into the bloodstream. From there, insulin helps to move that glucose into cells to be used for energy.
Why does blood sugar matter with diabetes?
With diabetes, blood sugar levels can be high. In the case of type 1 diabetes, the pancreas doesn’t make insulin or makes very little insulin. As a result, glucose from the blood can’t get into cells to be used for energy.
In type 2 diabetes, cells in the body don’t respond well to insulin; in addition, the pancreas stops making enough insulin to help regulate blood sugar.
High blood sugar is called hyperglycemia. If left untreated, this condition can lead to serious complications. These include:
Other problems caused by high blood sugar include foot problems, gum disease, skin issues, and hearing loss.
Short-term, untreated hyperglycemia can cause potentially life-threatening complications such as:
Both conditions require immediate medical treatment.
Fasting blood sugars
A fasting blood sugar is a blood sugar that is measured or checked after fasting. “Fasting” means not eating or drinking anything, except water, for at least eight hours.
If you have diabetes and check your blood sugar with a meter, your healthcare provider will likely ask you to check fasting blood sugars. Depending on your sleep schedule, this is a blood sugar check that you do first thing in the morning after you wake up, before you eat breakfast or drink your morning coffee.
For most people who have diabetes, the goal is a fasting blood sugar from 80 to 130 mg/dL. Fasting blood sugar in people who do not have diabetes should be from 70 to 99 mg/dL.
A fasting blood sugar higher than 130 mg/dL can mean that certain hormones are causing your blood sugar to be too high (called the dawn phenomenon). Other possible causes of high fasting blood sugars include not having enough insulin or rebound high blood sugar after having a low blood sugar during the night.
Read more: What Should Blood Sugar Be at Bedtime?
A fasting blood sugar below 80 mg/dL can mean that you’re taking too much diabetes medication (including insulin); other causes might be not eating enough, being more active than usual, or drinking alcohol without eating.
Post-meal blood sugars
Because food has a big impact on your blood sugar, it’s helpful to check your blood sugar after a meal if you have diabetes. This is called a post-meal or postprandial blood sugar check and is intended to capture the “peak” or highest blood sugar after eating.
The American Diabetes Association (ADA) suggests a target of less than 180 mg/dL for most nonpregnant adults one to two hours after the start of a meal. For people without diabetes, the goal is a blood sugar of less than 140 mg/dL.
A blood sugar that’s above 180 mg/dL after eating often means that your meal was too high in carbohydrates. For example, a dinner of pasta and Italian bread is more likely to cause a post-meal glucose “spike” compared with a meal of grilled fish, vegetables, and brown rice. But high post-meal blood sugars may also occur due to:
- Forgetting to take your diabetes medication
- Not taking enough diabetes medication
- Feeling ill or stressed
- Not doing your usual level of physical activity
An occasional high blood sugar after a meal is normal if you can pinpoint the cause. But repeated high post-meal blood sugars can be cause for concern and may indicate a need for cutting back on carbs and/or starting or adjusting diabetes medicine.
High blood sugar levels
For someone who has diabetes, hyperglycemia is usually considered to be a blood sugar of greater than 180 mg/dL one or two hours after eating.
As blood sugar climbs higher than 180 mg/dL, symptoms of hyperglycemia may appear. These include feeling very thirsty, needing to urinate often, fatigue, irritability, and blurred vision.
Many people with diabetes will start to experience hyperglycemia symptoms once blood sugar levels reach 250 mg/dL, although this can vary by person.
Blood sugars that reach 400 mg/dL or higher can indicate a risk for the two serious conditions mentioned earlier:
DKA occurs more commonly in people with type 1 diabetes, although it can affect those with type 2 diabetes, as well. Along with hyperglycemia and elevated ketones (chemicals produced by the liver when it breaks down fat), rapid breathing, fruity-smelling breath, nausea and vomiting, and stomach pain may appear.
DKA can quickly turn into a medical emergency. Treatment includes replacing fluids and electrolytes, and administering insulin.
HHS is a complication of type 2 diabetes and presents with very high blood sugars, extreme dehydration, and decreased alertness or even loss of consciousness. Treatment focuses on correcting dehydration, replacing electrolytes, and administering insulin intravenously.
Find out more in: What Is Considered High Blood Sugar?
Low blood sugar levels
Blood sugar levels fluctuate throughout the day in both people with and without diabetes. For those who have diabetes, the general goal is to aim to keep blood sugars within a range of 80 mg/dL to 180 mg/dL (or the range recommended by your healthcare team).
Sometimes blood sugars will go too low, meaning, below 70 mg/dL. This is called hypoglycemia. You might have symptoms that alert you to a low blood sugar, such as feeling shaky or lightheaded, or having a fast heartbeat.
Not everyone has symptoms when they’re low, so frequent blood sugar checking with a meter or, preferably, using CGM (continuous glucose monitoring) can help to identify when glucose levels are dropping and become too low.
If this happens, you’ll need to treat the low with a source of carbohydrates to raise your blood sugar to a safe level.
A blood sugar level that goes too low (usually, below 54 mg/dL) is called severe hypoglycemia and means that you need help from someone to treat the low and help you recover.
Severe hypoglycemia puts you at risk of passing out. If blood sugar stays low for too long, it can lead to seizures, coma, and rarely, death. Treatment may include receiving glucagon by injection or inhalation, or intravenous glucose.
Read more in: What Is Considered Low Blood Sugar?
Individualized blood sugar goals
The glucose goals listed in the table above are not necessarily appropriate for every person with diabetes. In fact, the ADA strongly recommends that glucose goals be adjusted, as needed, based on certain factors. These include:
- Age: Older adults who have functional or cognitive impairment, or very young children may need higher glucose goals for the sake of safety and simplicity. However, younger adults without diabetes complications may benefit from lower glucose goals.
- Health status: People with limited life expectancy or certain medical conditions often have higher glucose targets.
- Hypoglycemia risk: A person with hypoglycemia unawareness (the inability to detect the early signs of low blood glucose) or a history of severe hypoglycemia will likely have higher blood sugar goals.
- Pregnant women with diabetes: Glucose goals are generally much tighter before and during pregnancy to help minimize complications for the mother and baby.
Talk with your healthcare provider about your glucose goals and what makes sense for you.
A1c goals
An A1c test is a blood test that measures the average amount of glucose in the blood over the past 2 to 3 months. The result of this test is measured as a percentage. Other terms for A1c are hemoglobin A1c, HbA1c, glycated hemoglobin, and glycosylated hemoglobin.
An A1c test is often used to diagnose prediabetes or diabetes, but it’s also a key test to help you and your healthcare team manage your diabetes. The higher your A1c level, the higher your risk of developing complications.
A general A1c target for most people with diabetes, says the ADA, is less than 7 percent. In people without diabetes, the goal is less than 5.7 percent.
An A1c between 5.7 percent and 6.4 percent indicates prediabetes, a condition where your blood sugar levels are higher than normal, but not high enough to be considered type 2 diabetes.
Prediabetes means that you are at high risk for developing type 2 diabetes; fortunately, making lifestyle changes can help prevent or delay type 2 diabetes and other serious problems.
People with diabetes usually have their A1c checked two to four times a year. If you’re meeting your treatment goals, an A1c check twice a year may be sufficient. However, if you’re not meeting your treatment goals or if your treatment plan is changing, you may need an A1c check more often.
Individualized A1c goals
An A1c of less than 7 percent may not be appropriate for everyone. The ADA states that “less stringent A1c goals are appropriate for individuals with limited life expectancy and/or significant functional and cognitive impairments.”
As an example, an A1c goal of up to 8 percent may be recommended for an older adult or for someone who experiences severe or frequent hypoglycemia.
A lower A1c goal of, say, 6.5 percent could be appropriate for a younger person who is not having frequent low blood sugars. For pregnant women with diabetes, the “ideal” A1c goal is less than 6 percent.
Once again, there is no one-size-fits-all when it comes to A1c goals; you and your healthcare provider should decide, together, the best A1c goal for you.
Final thoughts
Knowing your blood sugar and A1c targets is important if you have diabetes. Your blood sugar levels and A1c test results help you and your healthcare team know how well your diabetes is managed.
While it’s completely normal to have blood sugars and an occasional A1c outside your target range, blood sugars that are consistently too high or too low, or an A1c result that is consistently high, is a sign that a course correction in your diabetes treatment plan is indicated.
Have an open dialogue with your physician or other members of your healthcare team; ask about your glucose and A1c goals and discuss factors that can help you get to your targets, including medication, diet, and physical activity.
[ad_2]
Source_link